Cancer affects all of humankind, but there are marked differences across local, national, and regional boundaries, particularly when considering specific tumour types rather than cancer as a whole. Epidemiological data on incidence of cancer and deaths caused by cancer vary enormously in coverage and quality between countries and regions worldwide, ranging from complete coverage by national cancer registries to population-based registries, or no available data at all on cancer occurrence. In the absence of data, inferences must be drawn from surrounding countries to provide the best estimate possible.
Among men, the five most common sites of cancer diagnosed in 2012 were lung (16.7% of the total), prostate (15%), colorectum (10%), stomach (85%), and liver (7.5%). Among women, the five most common incident sites of cancer were the breast (25.2% of the total), colorectum (9.2%), lung (8.9%), cervix (7.9%) and stomach (4.8%).
Among men, lung cancer had the highest incidence (34.2 per 100 000) and prostate cancer had the second highest incidence (31.1 per 1000 000). Among women, breast cancer had a substantially higher incidence (43.3 per 100 000) than any other cancer; the next highest incidence was colorectal cancer (14.3 per 100 000).
Cancer is a global problem. Of the roughly seven million cancer deaths that occur worldwide, approximately 70% of these are in low and middle-income countries. The majority of the 27 million new cancer cases and 17 million cancer deaths that will occur by 2020 will also occur in resource-limited nations. Further, the likelihood of death from a particular type of cancer differs drastically from country to country. A woman with breast cancer in a high-income country has, on average, a less than 25% chance of dying from her disease, while the same woman in a low-income country has close to 60% chance of death. Disparities in access to timely diagnosis, and high-quality treatment likely explain these extremely different odds in survival for the same disease.
Common misconceptions have held that cancer is a disease of the wealthy, while poorer nations struggle exclusively with communicable diseases. In reality, cancer is and has always been a real burden in low and middle-income countries. More people die of cancer than of HIV, TB, and malaria combined, and two thirds of these deaths are in the developing world. Further, as people live longer and communicable diseases are addressed, the burden of cancer in low and middle-income countries is rising. By 2030, cancer will be the leading cause of death in these settings causing over 10 million deaths.
Cancer incidence has been increasing in most regions of the world, but there are huge inequalities between rich and poor countries. Incidence rates remain highest in more developed regions, but mortality is relatively much higher in less developed countries due to a lack of early detection and access to treatment facilities. For example, in western Europe, breast cancer incidence has reached more than 90 new cases per 100 000 women annually, compared with 30 per 100 000 in eastern Africa. In contrast, breast cancer mortality rates in these two regions are almost identical, at about 15 per 100 000, which clearly points to a later diagnosis and much poorer survival in eastern Africa.
Until recently, cancer has been excluded from broader discussions of global health. International and local organizations alike have focused on preventive and simple curative therapies, mostly for infectious diseases. However, as the global health community has recognized the
growing burden of cancer and other complex, chronic diseases, more organizations have realized that resources must be dedicated to creating systems that can provide the entire breadth of health services. Leadership by the Union of International Cancer Control, the Global Taskforce for Cancer Care and Control, ministries of health and many local partners have supported efforts for access to comprehensive cancer care with a focus on low and middle-income countries and equitable access to healthcare as a human right.
References
B.W. Stewart, C.P. Wild (2014), World Cancer Report 2014. Lyon: World Health Organization/ International Agency for Research on Cancer.
World Health Organization/ International Agency for Research on Cancer (2013) Latest world statistics. Lyon: WHO/IARC Press Release, 12 December, 2013.
Global RT, 2017, Source: http://globalrt.org/about-cancer/
Cancer is an emerging public health problem in Africa. According to the International Agency for Research on Cancer (IARC), about 715,000 new cancer cases and 542,000 cancer deaths occurred in 2008 in Africa. These numbers are projected to nearly double (1.28 million new cancer cases and 970,000 cancer deaths) by 2030 simply due to the aging and growth of the population, with the potential to be even higher because of the adoption of behaviors and lifestyles associated with economic development, such as smoking, unhealthy diet, and physical inactivity.
Despite this growing burden, cancer continues to receive low public health priority in Africa, largely because of limited resources and other pressing public health problems, including communicable diseases such as acquired immune deficiency syndrome (AIDS)/human immunodeficiency virus (HIV) infection, malaria, and tuberculosis. It may also be in part due to a lack of awareness about the magnitude of the current and future cancer burden among policy makers, the general public, and international private or public health agencies.
Sub-Saharan Africa provides several contrasts with other world regions. Among women, this is the only region where cervical cancer is
equivalent to breast cancer in terms of incidence (each constitutes approximately a quarter of the total burden) and is the most common cause of cancer death in women (23.2% of the total). The incidence and mortality rates for cervical cancer are 34.8 and 22.5 per 100 000 respectively, the highest of any world region. Among men, prostate and liver cancers are the most common forms of incident cancer and causes of cancer death. Although the leading role of prostate cancer in the cancer incidence pattern in men is shared with most other world regions, this regions also has mortality rates comparable to incidence rates. The rates of 27.9 and 20.9 per 100 000 for prostate cancer incidence and mortality, respectively, stand in marked contrast to those in Europe (64.0 and 11.3 per 100 000, respectively) or North America (97.2 and 9.8 per 100 000, respectively), where incidence much higher but mortality is much lower. The importance of liver cancer in this region should be emphasized; it is the second most common cancer in men and the third most common cancer in women. Cervical and breast cancers in women and prostate and liver cancers in men are the only cancers with sex-specific incidence or mortality rates of more than 10 per 100 000, but the high rates of Kaposi Sarcoma is the third most common cancer in men and represents 9.2% incidence rate of 7.2% of all cancer diagnoses, with an incidence rate of 7.2 per 100 000. This reflects the very high regional level of HIV infection and associated cancer sequelae before the advent of highly active antiretroviral therapy. Cervical cancer and Kaposi sarcoma also make important contributions to the pattern of 5-year prevalence in the region.
References
American Cancer Society (2011), Cancer in Africa. Atlanta: American Cancer Society.
B.W. Stewart, C.P. Wild (2014), World Cancer Report 2014. Lyon: World Health Organization/ International Agency for Research on Cancer.
In Nigeria, cancer leads to over 72,000 deaths per annum (30924 for male and 40 647 for female). This number is set to increase given that there are 102,000 new cases of cancer every year. The estimated incidence for breast cancer is (27%), cervix uteri (14%), liver (12%), prostate (12%) and colorectum (4.1%). While estimated mortality for breast cancer is (20%), liver (16%), prostate (13%), cervix uteri (12%) and
colorectum (4.4%). Breast cancer is now the leading cancer death in Nigeria, while liver cancer is the second and prostate cancer is the third.
Incidence of cancer has been increasing in most regions of the world, but there are huge inequalities between developed and developing countries like Nigeria. Incidence rates remain highest in more developed regions, but mortality is relatively much higher in less developed countries due to a lack of early detection and access to treatment facilities. For example, WHO/IARC asserted that in Western Europe, breast cancer incidence has reached more than 90 new cases per 100 000 women annually, compared with 30 per 100 000 in eastern Africa. In contrast, breast cancer mortality rates in these two regions are almost identical, at about 15 per 100 000, which clearly points to a later diagnosis and much poorer survival in eastern Africa.
Over 70% of the cancer patients present late stages (III & IV) with few patients having access to the limited treatment facilities. More people are diagnosed of cancer at advanced stages because so many people in Nigeria believe that cancer is “white people’s disease”. While some strongly believe that cancer is usually sent to other people by magical power known as “juju” or a demonic attack and others believe that it is a punishment sent to humanity from the Supreme Being. Consequently, the women diagnosed with breast cancer would visit traditional healers and faith-based centres, where they believe that they can get cure. Some of the women gets incision on the affected breasts, brainwashed never to accept that they are battling with cancer; rather, they should rebuke and employ the “not my portion” exclamation. After, the series of visits to different traditional healers, they eventually reverse to the healthcare facility at a very advanced stage where only palliative care can be offered.
References
IARC/WHO POPULATION FACT SHEETS: NIGERIA https://gco.iarc.fr/today/fact-sheets-populations?population=566&sex=0
Adenipekun, A., Onibokun, A. Elumelu, T.N., Soyannwo, O.A. (2005). Knowledge and Attitudes of Terminally Ill Patients and Their Family To Palliative Care and Hospice Services in Nigeria. Nigeria Journal of Clinical Practice, June 2005, 8 (1): 19-22.
Report of workshop of National Headquarters of cancer Registry on National Cancer Control Programme (NCCP) for Nigeria, Dec 1992; 7-11.
The body is made up of trillions of living cells. Normal body cells grow, divide into new cells, and die in an orderly way. During the early years of a person’s life, normal cells divide faster to allow the person to grow. After the person becomes an adult, most cells divide only to replace worn-out or dying cells or to repair injuries.
Cancer begins when cells in a part of the body start to grow out of control. There are many kinds of cancer, but they all start because of out-of-control growth of abnormal cells.
Cancer cell growth is different from normal cell growth. Instead of dying, cancer cells continue to grow and form new, abnormal cells. Cancer cells can also invade (grow into) other tissues, something that normal cells cannot do. Growing out of control and invading other tissues are what makes a cell a cancer cell.
In most cases the cancer cells form a tumor. Some cancers, like leukemia, rarely form tumors. Instead, these cancer cells involve the blood and blood-forming organs and circulate through other tissues where they grow.
Cancer cells often travel to other parts of the body, where they begin to grow and form new tumors that replace normal tissue. This process is called metastasis. It happens when the cancer cells get into the bloodstream or lymph vessels of our body.
Not all tumors are cancerous. Tumors that aren’t cancer are called benign. Benign tumors can cause problems – they can grow very large and press on healthy organs and tissues. But they cannot grow into (invade) other tissues. Because they can’t invade, they also can’t spread to other parts of the body (metastasize). These tumors are almost never life threatening.
References
American Cancer Society (2013) Breast Cancer. Atlanta: American Cancer Society.
BREAST CANCER: What you need to know.
If you or a loved one has been diagnosed with breast cancer, it’s important to understand some basics: What is breast cancer and how does it happen?
You can learn about how breast cancer develops, how many people get breast cancer, and what factors can increase risk for getting breast cancer. You also can learn more about signs and symptoms to watch for and how to manage any fears you may have about breast cancer.
The term “breast cancer” refers to a malignant tumor that has developed from cells in the breast. Usually breast cancer either begins in the cells of the lobules, which are the milk-producing glands, or the ducts, the passages that drain milk from the lobules to the nipple. Less commonly, breast cancer can begin in the stromal tissues, which include the fatty and fibrous connective tissues of the breast. Over time, cancer cells can invade nearby healthy breast tissue and make their way into the underarm lymph nodes, small organs that filter out foreign substances in the body. If cancer cells get into the lymph nodes, they then have a pathway into other parts of the body. The breast cancer’s stage refers to how far the cancer cells have spread beyond the original tumor.
Breast cancer always happen as a result of genetic abnormality (a “mistake” in the genetic material). However, only 5-10% of cancers are due to an abnormality inherited from your mother or father. Instead, 85-90% of breast cancers are due to genetic abnormalities that happen as a result of the aging process and the “wear and tear” of life in general.
IS THERE BREAST CANCER IN NIGERIA?
Yes! You may have heard that breast cancer is “white people’s” disease or “rich people’s” disease. It is not true. Breast cancer is global burden and it can happen to anybody, black, white, whether rich or poor.
In Nigeria, 72,000 people die of cancer annually. This number is set to increase given that there are 102,000 new cases of cancer every year. The mortality incidence for breast cancer is (51%). It is
estimated that thirty(30) Nigerian women die every day from breast cancer.
WHO IS AT RISK OF BREAST CANCER?
Everybody is at risk of breast cancer including men, however, the following increases your risk of breast cancer:
- Being female
- Getting older
- Having an inherited mutation in the BRCA1 or BRCA2 breast cancer genes (speak to your doctor for clarification)
- Having a breast biopsy showing lobular carcinoma in situ (LCIS) or hyperplasia
- A family history of breast, ovarian or prostate cancer
- Having high breast density on a mammogram
- Having a personal history of breast or ovarian cancer
- Never having children
- Having first child after age 35
- Currently or recently using menopausal hormones (estrogen or estrogen plus progestin)
- Being overweight after menopause or gaining weight as an adult
- Starting menopause after age 55
- Having your first period before age 12
- Having more than one drink of alcohol per day
- Having high bone density
- Currently or recently using birth control pills
- Being exposed to large amounts of radiation, such as frequent X-rays in youth
Please note, risk factors do not cause breast, but they increase the chances that breast cancer may develop. Having many risk factors for breast cancer does not mean that you will get breast cancer. It means that your chances of getting the disease are higher than those who have fewer risk factors. Also, many women with breast cancer do not have any known risk factors aside from being female.
There are some risk factors that you can control and others you cannot. Remember; even if you do not have any of these risk factors you can still get breast cancer.
FACTORS TO REDUCE THE RISK OF BREAST CANCER
There are steps every person can take to help the body stay as healthy as possible, such as:
- Pass on that last call for alcohol (limit alcohol intake)
- Eating a balanced diet (intake fresh fruits and vegetables)
- Talk to both sides of your family to learn about your family health history
- Maintaining a healthy weight
- Quit smoking
- Get physical, and do regular exercise
- Limit menopausal hormone use
- Get screened: Breast self-exam, Clinical breast exam or mammogram, speak to your doctor
- Consider breastfeeding instead of formula feeding
While these may have some impact on your risk of getting breast cancer, they cannot eliminate the risk. Developing breast cancer is not your or anyone’s fault. Feeling guilty, or telling yourself that breast cancer happened because of something you or anyone else did, is not productive.
WHAT CAUSES HIGHER MORTALITY IN NIGERIA?
- Late diagnosis: Screening not widely available, even where available there is lack of awareness, even where people are aware, there’s still low utilisation of screening services;
- Seeking traditional medication when women develop symptoms.
- Lack of knowledge of suggestive symptoms.
- Inability to afford treatment.
SYMPTOMS: HOW DOES ONE KNOW IF THEY HAVE BREAST CANCER?
Breast cancer symptoms vary widely — from lumps to swelling to skin changes — and many breast cancers have no obvious symptoms at all. Symptoms that are similar to those of breast cancer may be the result of non-cancerous conditions like infection or a cyst.
Below are some symptoms of breast cancer:
- Change in size or shape
- A nipple turned inward into the breast (discharge, retraction, deviation)
- A lump or thickening in or near the breast or in the under arm
- Skin may be scaly, red or swollen
- It may have ridges, and appears as the skin of orange
- Abnormal Mammogram
- Breast pain
HOW IS BREAST CANCER DIAGNOSED?
If you find any symptoms mentioned above, please contact your doctor or a specialist immediately. Your doctor will ask you about your family and personal medical history. The doctor will do a clinical breast exam and recommend one or more of the following tests:
- Mammogram
- Ultrasound
- MRI Breast
- FNAC
Breast self-exam should be part of your monthly health care routine, and you should visit your doctor if you experience breast changes. If you’re over 40 or at a high risk for the disease, you should also have an annual mammogram and physical exam by a doctor. The earlier breast cancer is found and diagnosed, the better your chances of beating it.
Just as no two people are exactly alike, no two breast cancers are exactly the same, either. Your doctor will order a series of tests on the cancer and nearby tissues to create a “profile” of how the breast cancer looks and behaves. Some of these tests are done after the initial biopsy (removal of tissue sample for testing), others in the days and weeks after lumpectomy or mastectomy.
IS THERE ANY TREATMENT FOR BREAST CANCER?
Yes! Breast cancer is treatable if found early. There are two main types of breast cancer treatment: local and systemic.
Local Treatments are used to remove cancer from a limited (local) area such as the breast, chest wall and lymph nodes in the underarm to make sure it does not come back in that area. The following are Local Treatments:
- Surgery: these could be lumpectomy (conserving the breast by removing the cancerous lump/tumor) and Mastectomy (the surgical removal of the entire breast).
- Radiation therapy: the use of high-energy X-rays to destroy any cancer cells that may remain in the breast after surgery. This reduces the chance of recurrence.
Systemic Treatment: the goal of systemic treatment is to kill any cancer cells that may have spread from the breast to any other parts of the body. It includes treatments such as chemotherapy, hormone therapy and targeted therapy.
- Chemotherapy refers to anti-cancer drugs that are given to treat cancer. These drugs are used to kill or slow the growth of cancer cells that may be anywhere in the body. They are given to lower the risk of the cancer spreading in the future. It may be given before or after surgery.
- Hormone Therapy uses drugs to slow or stop the growth of hormone receptor-positive tumors by preventing the cancer cells from getting the hormones they need to grow.
- Targeted Therapy targets the inner workings of cancer cells. Targeted therapies go straight to the genes and proteins in cancer cells to stop their growth or spread. When certain cancer cells are blocked or stop working, the cancer cells cannot grow. As a result, cancer cells are affected by the treatment more than healthy cells.
Being diagnosed of BREAST CANCER is not a death sentence. At Project PINK BLUE, we are here to support you through your journey with cancer.
Call us: 08000CANCER.
References
American Cancer Society (2013) Breast Cancer. Atlanta: American Cancer Society.
BreastCancer.Org (2017). Your Breast Cancer Diagnosis. Source: http://www.breastcancer.org/symptoms/diagnosis Access: February 10, 2017 at 9:08 AM
WHAT IS ADVANCED BREAST CANCER?
Breast cancer begins when abnormal cancerous cells in the breast grow and multiply without stopping, creating a tumor. Breast cancer usually starts in the ducts or lobules of the breast.
Advanced breast cancer usually refers to metastatic breast cancer, also called Stage IV breast cancer or secondary breast cancer. Breast cancer that has spread locally in the area of the breast, but not to distant organs and tissues, is often referred to as “locally advanced breast cancer,” or Stage III breast
cancer. Given these various and sometimes inconsistent terms, if you or a loved one is diagnosed with advanced breast cancer, it’s important to discuss with your doctor specifically what stage it is and its other characteristics (eg, biology and where the cancer has spread). Knowing these details of a diagnosis can help you to understand important treatment decisions.
“Advanced cancer” in general often means that the cancer is “metastatic” ie, has spread from where it started to distant parts of the body.
Breast Cancer is the most common cancer in women with nearly 1.7. million new cases diagnosed each year worldwide.
In Nigeria, cancer leads to 72,000 deaths per annum. This number is set to increase given that there are 102,000 new cases of cancer every year. The mortality incidence ratio for breast cancer is 0.51 (51%); this is partly because about 70% of these cancer patients present late stages (III & IV) with few patients having access to the limited treatment facilities and over 70% have pain.
HOW IS BREAST CANCER STAGED?
Breast cancer is divided into five main stages, 0 through IV. The stages are based on wether the cancer is invasive or not, the size of the tumor, the number of lymph nodes involved, and if the cancer has spread to other parts of the body.
Stage 0
Stage 0 is used to describe non-invasive breast cancers, such as DCIS (ductal carcinoma in situ). In stage 0, there is no evidence of cancer cells or non-cancerous abnormal cells breaking out of the part of the breast in which they started, or getting through to or invading neighboring normal tissue.
Stage I
Stage I describes invasive breast cancer (cancer cells are breaking through to or invading normal surrounding breast tissue).
Stage II
Stage II describes invasive breast cancer with 2-5 cm and or invasion in 1-3 axillary lymphnodes
Stage III
Stage III describes invasive breast cancer in which either: no tumor is found in the breast or the tumor may be any size; cancer is found in 4 to 9 axillary lymph nodes or in the lymph nodes near the breastbone (found during imaging tests or a physical exam) or the tumor may be any size and has spread to the chest wall and/or skin of the breast and caused swelling or an ulcer and there may be no sign of cancer in the breast or, if there is a tumor, it may be any size and may have spread to the chest wall and/or the skin of the breast and the cancer has spread to 10 or more axillary lymph nodes.
Stage IV
Stage IV describes invasive breast cancer that has spread beyond the breast and nearby lymph nodes to other organs of the body, such as the lungs, distant lymph nodes, skin, bones, liver, or brain.
You may hear the words “advanced” “secondary” and “metastatic” used to describe stage IV breast cancer. Cancer may be stage IV at first diagnosis or it can be a recurrence (distant recurrence) of a previous breast cancer that has spread to other parts of the body.
WHAT IS METASTASIS AND HOW DOES IT HAPPEN?
Metastasis means the spread of cancer cells to other parts of the body. Cancer cells can break away from a primary tumor and enter the bloodstream or lymphatic system (the system that produces, stores, and carries the cells that fight infections). This is how cancer cells spread to other parts of the body.
When cancer cells spread and form a new tumor in a different organ, the new tumor is a metastatic tumor. The cells in the metastatic tumor come from the original tumor. This means, for example, that if breast cancer spreads to the lungs, the metastatic tumor in the lung is made up of cancerous breast cells (not lung cells). In this case, the disease in the lungs is metastatic breast cancer (not lung cancer).
The most common sites of metastasis from solid breast cancer tumors are the lungs, bones, and liver. However, cancer can spread to other parts of the body as well.
Under a microscope, metastatic breast cancer cells generally look the same as the cancer cells in the breast, so you should consult an oncologist who specializes in the treatment of breast cancer regardless of where the cancer has spread. Sometimes after this first appointment and if there is a need for a special
treatment of metastasis in particular organs the breast cancer specialist can ask for advice to a neurosurgeon or an orthopedic surgeon about surgery in a brain or bone metastasis that will benefit from surgery.
HOW DOES A DOCTOR KNOW WHETHER A CANCER IS PRIMARY OR METASTATIC TUMOR?
To determine whether a tumor is primary or metastatic, a pathologist (a doctor who identifies diseases by studying cells and tissues under a microscope) examines a sample of the tumor. In general, cancer cells look like abnormal versions of cells in the tissue where the cancer first appeared. Using specialized diagnostic tests, a pathologist is often able to tell where the cancer cells came from. Doctors may determine the primary site of cancer in a few ways. They may look for markers, which are a diagnostic indication that disease may develop. They may also look for antigens, a substance that causes the immune system to have a specific immune response.
Metastatic cancer may be found before or at the same time as the primary tumor, or months or years later. When a new tumor is found in a patient who has been treated for cancer in the past, it is more frequently a a metastasi
WHAT ARE THE SYPTOMS OF A METASTATIC BREAST CANCER?
Some people with metastatic cancer do not have symptoms. Their metastases may be found by X-rays and other tests. These tests include magnetic resonance imaging (MRI), computed tomography (CT scan), and positron emission tomography (PET scan), which are performed usually when patients have specific complaints during follow-up appointments.
When symptoms of metastatic cancer occur, the type and frequency of the symptoms will depend on the size and location of the metastasis. For example, cancer that spreads to the bones can cause pain and can lead to bone fractures. Shortness of breath may be a sign of lung involvement. Abdominal swelling or jaundice (yellowing of the skin) can indicate that cancer has spread to the liver.
Sometimes a person’s primary cancer is discovered only after the metastatic tumor causes symptoms.
WHAT IS RERCURRENCE?
Recurrent breast cancer is cancer that has come back in the same or opposite breast or chest wall after a period of time when the cancer couldn’t be detected – this is called a local
recurrence. When then cancer returns in the lymphnodes of the axilla or around the collarbone it is called a regional recurrence. When the cancer spreads to other parts of the body, it is called a distant recurrence or metastatic breast cancer. Almost everyone who had cancer fears that one day the cancer will come back, or recur. Keep in mind that a local or locorregional recurrence of breast cancer has treatment and even a distante recurrence – metastatic (advanced) disease is NOT hopeless. Many women continue to live long, productive lives with breast cancer after recurrences. It is also likely that your experience with treatment this time will be somewhat different from last time. There are so many options for your care and so many ways to chart your progress as you move through diagnosis, treatment, and beyond.
When you had surgery to remove the original breast cancer, your surgeon removed all the cancer that could be seen and felt. But tests for cancer aren’t sensitive enough to detect a tiny group of single cancer cells. These isolated cells may survive radiation therapy and chemotherapy aimed at preventing recurrence. Even a single cell that escaped treatment may be able to spread and grow into a tumor.
Being diagnosed with recurrent or metastatic breast cancer can be overwhelming. Women experiencing a recurrence may find themselves back on the emotional rollercoaster they thought they got off of after initial treatment. Other women may be angry, scared, stressed, outraged, and depressed. Some may question the treatments they had or may be mad at their doctors or themselves for not being able to beat the disease. Still other women may deal with diagnosis of recurrent or metastatic breast cancer in a matter-of-fact way. There is no right or wrong way to come to terms with the diagnosis. You need to do and feel what is best for you and your situation.
There are two important things to remember about diagnoses of recurrent and “metastatic” advanced breast cancer:
- You are not alone. More and more people are living life to the fullest while being treated for advanced-stage cancer.
- You can have confidence that there are a wide variety of available treatment choices. There are many treatment options for advanced breast cancer, and new medicines are being tested every day. While recurrent or metastatic breast cancer
may not go away completely, treatment may control it for a number of years. If one treatment stops working, there usually is another you can try. The cancer can be active sometimes and then go into remission at other times. Many different treatments — alone, in combination, or in sequence — are often used. Breaks in treatment can make a big difference when the disease is under control and you are feeling good.
Are You In Need Of Palliative Care Or Any Other Support?
We can connect you. Call our patient navigators now: 0800CANCER (0800226237) for free support.
References
http://www.advancedbreastcancercommunity.org/advanced-breast-cancer/?accordion=oooooo
http://www.breastcancer.org/symptoms/diagnosis/staging#stage0
GLOBOCAN. 2012 Breast Cancer Incidence and Mortality Worldwide. Available at: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx. Accessed on January 12, 2015.
Adenipekun, A., Onibokun, A. Elumelu, T.N., Soyannwo, O.A. (2005). Knowledge and Attitudes of Terminally Ill Patients and Their Family To Palliative Care and Hospice Services in Nigeria. Nigeria Journal of Clinical Practice, June 2005, 8 (1): 19-22.
Report of workshop of National Headquarters of cancer Registry on National Cancer Control Programme (NCCP) for Nigeria, Dec 1992; 7-11.
Acknowledgement: Thanks to our Scientific Committee for compiling this handbook and Special Thanks to Union for International Cancer Control (UICC) & Pfizer Oncology whose support brought this handbook to you.
What is cervix?
The cervix is the lowest part of the uterus (womb) that connects the uterus to the vagina.
Cancer of the cervix is an abnormal growth in the cervix consisting of cells that have become abnormal and are growing uncontrollable. This growth can invade the uterus, vagina, urinary tract, and other surrounding tissues, as well as spread to other parts of the body like and lungs through blood or lymph.
Cervical cancer takes a long time to progress hence, if caught early it can be treated
Who does it affect?
Cervical cancer is disease that obviously affects women only. It occurs in all parts of the world. Cervical cancer used to be a huge problem in developed countries but this is no longer the case thanks to screening and vaccination. Presently, almost 9 out of 10 cervical cancer deaths occur in less developed regions of the world.
Cervical Worldwide
Every year, cervical cancer kills more than 250 000 women, and 85% of these deaths occur in low- and middle-income countries. Cervical cancer is the fourth most common cancer in women worldwide, but most of these deaths could be prevented with adequate prevention measures, such as vaccination of girls against human papillomavirus (HPV) and screening programmes to detect and treat precancerous lesions.
Cervical Cancer in Nigeria
Cervical cancer is the fourth most common cancer in women worldwide, but actually the second most common cancer in women in Nigeria after breast cancer. It is also the most common gynaecological (or female reproductive) cancer in Nigeria. There are over 14,000 new cases and over 8,000 deaths due to cervical cancer occurring annually in Nigeria, making it the second most common cause of cancer deaths in Nigerian women. However, more than half of women diagnosed with cervical cancer in Nigeria die making it the most deadly cancer in Nigerian women. This high mortality is mostly driven by late diagnosis at which time it cannot be cured.
What causes higher mortality in Nigeria?
- Late diagnosis: Screening not widely available, even where available there is lack of awareness, even where people are aware, there’s still low utilisation of screening services;
- Seeking traditional medication when women develop symptoms.
- Lack of knowledge of suggestive symptoms.
- Inability to afford treatment.What leads to cervical cancer?Cervical cancer is one of the few cancers for which a specific cause is known. The chief cause of cervical cancer is a virus called Human Papilloma Virus (HPV). HPV is a sexually transmissible. Most people acquire HPV infection shortly after becoming sexually active because it is a very common sexually transmissible infection (8 out of 10 women will acquire the infection at some point in their life). There are two categories (serotypes) of the virus that are responsible for the majority of cervical cancers. HPV is also associated with cancer of the vagina/vulva, mouth, throat (oropharynx), penis. Other serotypes of HPV that do not cause cancer are responsible for causing genital warts.
However, majority of HPV infection cause no problems, go unnoticed and resolve on their own. The few that persist cause a chronic infection and some pre-cancerous changes in the cervix that can eventually lead to cervical cancer if left untreated. The time period between HPV infection and eventual development of cervical cancer can be as long as 10 to 20 years. Therefore, providing a window period where development of cervical cancer can be prevented.
What are the risk factors for cervical cancer?
Since HPV is a sexually transmissible infection some of the risk factors are
- becoming sexually active at an early age
- having multiple sexual partners
Other important risk factors for development of cervical cancer include
- high parity (i.e having had many pregnancies and deliveries),
- cigarette smoking,
- HIV
- Taking oral contraceptive pills for a long time
How does one know if they have cervical cancer?
In its early stages, cervical cancer has no symptoms, therefore one does not feel anything. That is why it is such a silent killer. The pre-cancerous cervical changes also do not cause any symptoms. It can only be detected through regular check-ups called screening.
As it advances into later stages cervical cancer causes
- Abnormal bleeding like post-coital bleeding (i.e bleeding after sexual intercourse)
- Vaginal discharge, sometimes foul-smelling
- Pain like pelvic pain or lower back pain
Other symptoms like
- weight loss
- loss of appetite,
- easy fatiguability
This is why screening for cervical cancer is very important.
Screening for cervical cancer
Screening tests are tests carried out to detect the presence of a disease even before it has occurred. Therefore cervical cancer screening is done to detect the presence of HPV disease or pre-cancerous changes in the cervix or even early stages of cervical cancer.
This allows for treatment to be given such that one does not develop cervical cancer.
There are a number of methods for cervical cancer screening these include
- Pap smear
- Colopsocopy
- HPV testing
- VIA (Visual inspection with Acetic acid) and VILI (Visual Inspection with Lugol’s Iodine)
When pre-cancerous abnormalities are detected in the cervix, a number of treatment options are available which include
- Cryotherapy
- Cone biopsy
- LEEP
How is cervical cancer treated?
Cervical cancer is curable if diagnosed early and treated appropriately.
Treatment option include surgery, chemotherapy, radiation therapy or a combination of these. Adjunctive treatments like pain management, nutritional support and treatment of anaemia are also offered as needed. Treatment depends on the stage of the cancer (how advanced it is).
In early stages surgical operation is done to remove the uterus (including the cervix) and or the ovaries.
Can cervical cancer be prevented?
Cervical cancer can be prevented through two major ways.
- Vaccination against HP -Since the majority of cervical cancers are directly caused by infection with HPV oncogenic serotypes 16 and 18, vaccination against these is a highly effective way of preventing cervical cancer. This is one of the main methods of control that has reduced cervical cancer incidence in developed countries. Vaccination is done for pre-adolescent girls who are yet to become sexually active. As described above, screening allows for pre-cancerous changes in the cervix to be detected and treated so that they do not progress to cancer.
- Screening – As described above, screening allows for pre-cancerous changes in the cervix to be detected and treated so that they do not progress to cancer.
Cervical cancer vaccine
There are currently two vaccines available for HPV, CervarixR which is active against the oncogenic HPV serotypes 16 and 18 and GardasilR which is active against the two oncogenic serotypes as well as two serotypes which cause genital warts (6 and 11).
They are currently not part of our national immunisation schedule. Therefore, they presently have to be purchased by individuals.
References
GLOBOCAN/IARC, 2012. Fact sheets by cancer, Cervical cancer. Available at http://globocan.iarc.fr/old/FactSheets/cancers/cervix-new.asp
GLOBOCAN/IARC, 2012. Fact Sheets by Population, Nigeria. Available at http://globocan.iarc.fr/Pages/fact_sheets_population.aspx
World Health Organisation, (2014). Comprehensive cervical cancer control: a guide to essential practice (C4GEP). Available at http://apps.who.int/iris/bitstream/10665/144785/1/9789241548953_eng.pdf
World Health Organization/IARC (2017). Affordable vaccines key to scale up HPV vaccination and prevent thousands of avoidable cervical cancers. Press Release, 2 February, 2017, Lyon.
Prostate cancer begins when cells in the prostate gland start to grow uncontrollably. The prostate is a gland found only in males. It makes some of the fluid that is part of semen.
The prostate is below the bladder and in front of the rectum. The size of the prostate changes with age. In younger men, it is about the size of a walnut, but it can be much larger in older men.
Just behind the prostate are glands called seminal vesicles that make most of the fluid for semen. The urethra, which is the tube that carries urine and semen out of the body through the penis, goes through the center of the prostate.
TYPES OF PROSTATE CANCER
Almost all prostate cancers are adenocarcinomas. These cancers develop from the gland cells (the cells that make the prostate fluid that is added to the semen).
Other types of prostate cancer include:
- Sarcomas
- Small cell carcinomas
- Neuroendocrine tumors (other than small cell carcinomas)
- Transitional cell carcinomas
These other types of prostate cancer are rare. If you have prostate cancer it is almost certain to be an adenocarcinoma.
Some prostate cancers can grow and spread quickly, but most grow slowly. In fact, autopsy studies show that many older men (and even some younger men) who died of other causes also had prostate cancer that never affected them during their lives. In many cases neither they nor their doctors even knew they had it.
PROSTATE CANCER IN NIGERIA
The estimated incidence for prostate cancer is (12%) and estimated mortality prostate (13%). Prostate cancer is the third leading cancer death in Nigeria.
RISK FACTORS OF PROSTATE CANCER
Age
Age is the most significant risk factor for prostate cancer. Your risk increases as you get older. Prostate cancer is quite rare in men under 50.
Remember, this is a lifetime risk and involves men who get prostate cancer at any age, up to 85 or older. Your risk when you are younger is much lower than 1 in 8.
A family history of cancer
A family history means that you have someone in your family who has cancer. Generally speaking, if you have a father or brother diagnosed with prostate cancer you are 2 to 3 times more likely to get prostate cancer yourself, compared to the average man. The age that your relative is diagnosed with prostate cancer may also be a factor. If they were diagnosed before the age of 60, this increases your risk by slightly more than if they were diagnosed after the age of 60. If you have more than one first degree relative diagnosed with prostate cancer (at any age) your risk is about 4 times that of the general population.
Genes
Scientists are working on identifying other genes that may increase the risk of prostate cancer. In 2008, Cancer Research UK scientists identified 7 gene changes that increase the risk of prostate cancer. In the future, they may develop a test, to see if men are carrying any of these genes.
People with Lynch syndrome have inherited faulty genes that increase their risk of developing certain cancers. Researchers have found that men with Lynch syndrome may have a higher risk of prostate cancer than men in the general population.
Ethnicity
Prostate cancer is more common in black Caribbean and black African men than in white or Asian men. In the UK, black African and black Caribbean men have double the risk of developing prostate cancer compared to white men. Asian men have half the risk of white men.
A previous cancer
Men who have had certain cancers in the past, may have a slightly increased risk of getting prostate cancer. Studies have shown an increase in risk for men who have had kidney cancer, bladder cancer, lung cancer, thyroid cancer and melanoma skin cancer.
Calcium in your diet
We still don’t fully understand how diet affects prostate cancer risk. Several factors have been studied. Some studies show that men who have diets high in calcium may have a higher risk of prostate cancer.
Height and body weight
Research has shown that taller men have a higher risk than shorter men of getting faster growing (high grade) prostate cancer, or prostate cancer that has spread.
Being overweight for your height (obese) may also affect your risk. Some studies have found that having a high body mass index (BMI) increases your risk of dying from prostate cancer or being diagnosed with high grade prostate cancer. But it lowers your risk of getting localised prostate cancer. Doctors think that these results may partly be because it is harder to diagnose and treat prostate cancer in obese men.
Hormones
Hormone levels may or may not play a part in the risk of developing prostate cancer. The prostate gland is a sex organ. It produces a liquid that is mixed with sperm to make semen. Testosterone is a sex hormone produced by the testicle and the prostate gland needs testosterone to work. It was thought in the past that having higher levels of testosterone in the blood may increase the risk of prostate cancer. But, in 2008 an analysis of 18 separate studies found no link between levels of sex hormones and prostate cancer risk.
Vasectomy
A large study reported in the USA in 2014. It showed a small increased risk of prostate cancer in men who have had a vasectomy. Vasectomy is a procedure for male sterilisation and permanent birth control. Two other large studies in 1993 also found a small increase in risk but other studies have not shown an increased risk. It seems likely that vasectomy does increase the risk of prostate cancer but the increase in risk is very small.
Cadmium
Cadmium is a natural metal in the environment. Small amounts can be found in our foods. There is limited evidence that a diet which contains a high amount of cadmium may increase your risk of getting prostate cancer.
Inflammation of the prostate
Inflammation of the prostate is called prostatitis. A meta-analysis published in 2013 combined the information from 20 studies looking at prostate cancer risk and prostatitis. It found that men with prostatitis had a higher risk of prostate cancer. But the meta-analysis included low quality research studies. The results from another higher quality study did not find a link between prostatitis
and prostate cancer. So we need more research before we know whether prostatitis increases your risk of prostate cancer
Symptoms of prostate Cancer
As men get older their prostate gland often enlarges. This is usually not due to cancer. It is a condition called benign prostatic hyperplasia (BPH). BPH does not usually develop into cancer but an enlarged prostate may sometimes contain areas of cancer cells.
Very early prostate cancer generally does not cause any symptoms at all. Many prostate cancers start in the outer part of the prostate gland, away from the urethra. If a tumour is not large enough to put much pressure on the tube that carries urine out of the body (the urethra), you may not notice any effects from it.
The symptoms of growths in the prostate are similar whether they are non cancerous (benign) or cancerous (malignant).
The symptoms include
-Having to rush to the toilet to pass urine
-Passing urine more often than usual, especially at night
-Difficulty passing urine, including straining to pass it or stopping and starting
-A sense of not being able to completely empty the bladder
-Very rarely you may get Pain when passing urine
-Blood in the urine or semen
Prostate Cancer Screening
Screening is testing to find cancer in people before they have symptoms. For some types of cancer, screening can help find cancers at an early stage, when they are likely to be easier to treat.
Prostate cancer can often be found before symptoms arise by testing the amount of prostate-specific antigen (PSA) in a man’s blood. Another way to find prostate cancer is the digital rectal exam (DRE), in which the doctor puts a gloved, lubricated finger into the rectum to feel the prostate gland. These tests are described in more detail in Prostate Cancer Prevention and Early Detection.
If the results of either one of these tests are abnormal, further testing is often done to see if a man has cancer. If prostate cancer is found as a result of screening with the PSA test or DRE, it will probably be at an earlier, more treatable stage than if no screening were done.
There is no question that screening can help find many prostate cancers early, but there are still questions about whether the
benefits of screening outweigh the risks for most men. There are clearly both pros and cons to the prostate cancer screening tests in use today.
At this time, the American Cancer Society (ACS) recommends that men thinking about getting screened for prostate cancer should make informed decisions based on available information, discussion with their doctor, and their own views on the possible benefits, risks, and limits of prostate cancer screening.
References
http://www.cancer.org/cancer/prostatecancer/detailedguide/prostate-cancer-what-is-prostate-cancer
LIVER CANCER & HEPATITIS IN NIGERIA
Liver cancer is the second leading cancer death in Nigeria and it is associated with viral hepatitis, which is virtually unknown to the general public, including some fractions of health-care providers. Complications of viral hepatitis infections such as cirrhosis of the liver, liver cancer and liver failure associated with liver cancer affect mostly people at their prime of life. Epidemiological study reveals that 1 in every 8 persons in Nigeria is living with viral Hepatitis and about 22 million Nigerians are estimated to be infected with either HBV or HCV. 90-95% of Mother to Child Transmission of viral hepatitis ends in chronic hepatitis and in the absence of treatment, 15 – 40% of persons living with viral hepatitis will develop liver cirrhosis and/or liver cancer.
Economically, treatment of hepatitis is expensive usually in millions of naira, 60% and 33% of liver cancer cases in developing countries are caused by Hepatitis B and Hepatitis C respectively.
Over the years there have been series of information dissemination through different avenues to the people on the importance of vaccination especially polio but little emphasis has been focused on
cancer prevention through vaccination. And despite the resources available, preventable diseases such as cervical and liver cancer still constitute health risks and deaths among the people. This is so due to insufficient of proper channel of information or outright misinformation.
At Project PINK BLUE, we are using the World Immunization Week (WIW) to educate Nigerians on the need to vaccinate themselves against Hepatitis, thereby reducing their risk of liver cancer. Please click here to learn more about WIW.
LIVER CANCER
What is liver cancer?
Cancer can start any place in the body. Liver cancer starts in the liver. It starts when cells in the liver grow out of control and crowd out normal cells. This makes it hard for the body to work the way it should.
Cancer cells can spread to other parts of the body. Cancer cells in the liver can sometimes travel to the bone and grow there. When cancer cells do this, it’s called metastasis (pronounced meh-TAS-tuh-sis). To doctors, the cancer cells in the new place look just like the ones from the liver.
Cancer is always named for the place where it starts. So when liver cancer spreads to the bone (or any other place), it’s still called liver cancer. It’s not called bone cancer unless it starts from cells in the bone.
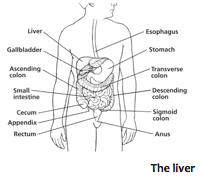
The liver
The liver makes bile to help the body use food. It also cleans the
blood and helps blood clot.
Are there different kinds of liver cancer?
There are many types of liver cancer. Some are very rare. Your doctor can tell you more about the type you have.
The most common kind is called hepatocellular carcinoma (heh-PA-toh-SEL-yoo-ler CAR-sih-O-muh). Sometimes it’s called HCC for short. It starts in the cells that make up the liver.
Some rare types of liver cancer are:
- Angiosarcoma (pronounced AN-jee-o-sar-KO-muh)
- Hemangiosarcoma (pronounced hee-MAN-jee-oh-sar-KOH-muh)
These start in the cells lining the blood vessels of the liver. They often grow quickly.
Secondary liver cancer
Most of the time when cancer is found in the liver it didn’t start there. It really spread there from somewhere else in the body. Because the cancer has spread from where it started, it’s called a secondary liver cancer. So, cancer that started in the lung and spreads to the liver is called lung cancer with spread to the liver, not liver cancer. This cancer would be treated like lung cancer, not liver cancer.
How does the doctor know I have liver cancer?
Tests that may be done
Liver cancer often doesn’t cause signs and symptoms until it has spread.
Some symptoms of liver cancer are unplanned weight loss, don’t feel like eating, feeling full after a small meal, belly pain and swelling, and itchy, yellow skin. The doctor will ask you questions about your health and do a physical exam.
If signs are pointing to liver cancer, more tests may be done. Here are some of the tests you may need:
Ultrasound: For this test, a small wand is moved around on your skin. It gives off sound waves and picks up the echoes as they bounce off tissues. The echoes are made into a picture on a computer screen. This test is often the first test used to look at the liver.
CT or CAT scan: Uses x-rays to make detailed pictures of your body. CT scans can show the size, shape, and place of any tumors in the liver or near it.
MRI: Uses radio waves and strong magnets instead of x-rays to make detailed pictures. MRI scans can help know if tumors in the liver are cancer. They can also be used to look at blood vessels in
and around the liver. They can help find out if liver cancer has spread.
Lab tests: Blood tests can check a protein called AFP (alpha-fetoprotein). AFP is often very high in people with liver cancer. Other blood tests can also help find out how well the liver is working.
Liver biopsy
In a biopsy (BY-op-see), the doctor takes out a small piece of tissue where the cancer seems to be. The tissue is checked for cancer cells.
There are many types of biopsies. Ask your doctor what kind you will need. Each type has pros and cons. The choice of which type to use depends on your own case.
Sometimes MRI or CT scans clearly show liver cancer and a biopsy isn’t needed.
Grading liver cancer
The cancer cells in the biopsy sample will be graded. This helps doctors predict how fast the cancer is likely to grow and spread. Cancer cells are graded based on how much they look like normal cells. Grades 1, 2, and 3 are used. Cells that look very different from normal cells are given a higher grade (3) and tend to grow faster. Ask the doctor to explain the grade of your cancer. The grade helps the doctor decide which treatment is best for you.
How serious is my cancer?
If you have liver cancer, the doctor will want to find out how far it has spread. This is called staging. You may have heard other people say that their cancer was “stage 1” or “stage 2.” Your doctor will want to find out the stage of your cancer to help decide what type of treatment is best for you.
The stage describes the growth or spread of the cancer through the liver. It also tells if the cancer has spread to other organs of your body that are close by or farther away.
Your cancer can be stage 1, 2, 3, or 4. The lower the number, the less the cancer has spread. A higher number, like stage 4, means a more serious cancer that has spread beyond the liver. Be sure to ask the doctor about the cancer stage and what it means for you.
What kind of treatment will I need?
There are many ways to treat liver cancer, but the main types of treatment are surgery, tumor ablation, radiation, targeted therapy, and chemotherapy. Many times more than one kind of treatment is
used.
The treatment plan that’s best for you will depend on:
- The stage and grade of the cancer
- The chance that a type of treatment will cure the cancer or help in some way
- Your age
- Other health problems you have
- Your feelings about the treatment and the side effects that come with it
Surgery for liver cancer
Surgery (SUR-jur-ee) is the only way to try to cure liver cancer. Surgery can be done to take out the part of the liver with the tumor or to do a liver transplant. Talk to the doctor about the kind of surgery planned and what you can expect.
Side effects of surgery
Any type of surgery can have risks and side effects. Be sure to ask the doctor what you can expect. If you have problems, let your doctors know. Doctors who treat liver cancer should be able to help you with any problems that come up.
Tumor ablation for liver cancer
Tumor ablation (a-BLAY-shun) destroys the tumor without taking it out. There are a number of ways to do this, such as heating the tumor with radio waves or microwaves, freezing the tumor, or killing the tumor by putting alcohol in it. Talk to the doctor about the planned treatment and what you can expect.
Radiation treatments
Radiation (pronounced RAY-dee-A-shun) uses high-energy rays (like x-rays) to kill cancer cells. There are different kinds of radiation. It can be aimed at the liver from a machine outside the body. This is called external beam radiation.
Radiation treatment can also be done by using a needle to put small radioactive beads into a large blood vessel in the liver (called the hepatic artery). This is called radioembolization (RAY-dee-oh-EM-boh-lih-ZAY-shun).
Side effects of radiation treatments
If your doctor suggests radiation treatment, talk about what side effects might happen. Side effects depend on the type of radiation that’s used. The most common side effects of radiation are:
- Skin changes where the radiation is given
- Feeling very tired (fatigue, which is pronounced fuh-TEEG)
Most side effects get better after treatment ends. Some might last longer. Talk to your doctor about what you can expect.
Targeted therapy for liver cancer
Targeted therapy drugs are newer treatments that may be used for certain types of liver cancer. These drugs affect mainly cancer cells and not normal cells in the body. They may work even if other treatment doesn’t. They come as pills that you take at home. These drugs have different side effects than chemo and they are often not as bad.
Chemo
Chemo (pronounced KEY-mo) is the short word for chemotherapy (pronounced KEY-mo-THAIR-uh-pee) – the use of drugs to fight cancer. The drugs may be given into a vein. These drugs go into the blood and spread through the body. Chemo is given in cycles or rounds. Each round of treatment is followed by a break. Chemo may be used to treat liver cancer, but it doesn’t work as well as other treatments for liver cancer.
Side effects of chemo
Chemo can make you feel very tired, sick to your stomach, and cause your hair to fall out. But these problems go away after treatment ends.
There are ways to treat most chemo side effects. If you have side effects, talk to your cancer care team so they can help.
What about other treatments that I hear about?
When you have cancer you might hear about other ways to treat the cancer or treat your symptoms. These may not always be standard medical treatments. These treatments may be vitamins, herbs, special diets, and other things. You may wonder about these treatments.
Some of these are known to help, but many have not been tested. Some have been shown not to help. A few have even been found to be harmful. Talk to your doctor about anything you’re thinking about using, whether it’s a vitamin, a diet, or anything else.
Questions to ask the doctor
- Why do you think I have cancer?
- What tests will I need to have?
- Do you know the stage of the cancer?
- What treatment do you think is best for me?
- What side effects could I have from these treatments?
- What should I do to be ready for treatment?
- Is there anything I can do to help the treatment work better?
- What do I need to do next?
What will happen after treatment?
You’ll be glad when treatment is over. For years after treatment ends, you will see your cancer doctor. Be sure to go to all of these follow-up visits. Your doctor will ask about any symptoms that you might have and you will have exams, blood tests, and maybe other tests done to see if the cancer has come back.
Your visits may be every 3 to 6 months for the first 2 years, then every 6 to 12 months. Then, the longer you’re cancer-free, the less often the visits are needed. After 5 years, they may be done once a year.
Having cancer and dealing with treatment can be hard, but it can also be a time to look at your life in new ways. You might be thinking about how to improve your health.
You can’t change the fact that you have cancer. What you can change is how you live the rest of your life – making healthy choices and feeling as good as you can.
REFERENCES
Bosman F. Carneiro F, Hruban R, Theise ND, eds (2010). WHO Classification of Tumours of the Digestive System, 4th ed. Lyon: IARC
McGlynn KA, London WT (2011). The global epidemiology of hepatocellular carcinoma: present and future. Clin Liver Dis, 15: 223-243, vii –x. http://dx.doi.org/10.1016/j.cld.2011.03.006 PMID:21689610.
American Cancer Society (2016) Liver Cancer. Access: March, 17th 2017, Source: https://www.cancer.org/cancer/liver-cancer.html
Colon cancer, which affects men and women, it is one of the most common cancer globally. It is approximated that 49,190 colorectal deaths occur in Nigeria in 2016. Colorectal cancer is the third most common cancer in Nigerian men (after prostate and liver cancer) and the fourth most common cancer in Nigerian women (after breast, cervical and liver cancer).
What is colon or rectum cancer?
Cancer can start any place in the body. Cancer that starts in the colon or rectum is often called colorectal cancer. It starts when cells in the colon or rectum grow out of control and crowd out normal cells. This makes it hard for the body to work the way it
should.
Cancer cells can spread to other parts of the body. Cancer cells in the colon or rectum can sometimes travel to the liver and grow there. When cancer cells do this, it’s called metastasis (pronounced meh-TAS-tuh-sis). To doctors, the cancer cells in the new place look just like the ones from the colon or rectum.
Cancer is always named for the place where it starts. So when colorectal cancer spreads to the liver (or any other place), it’s still called colorectal cancer. It’s not called liver cancer unless it starts from cells in the liver.
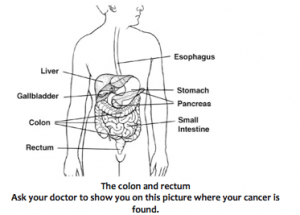
The colon and rectum
Colon cancer starts in the colon, and rectal cancer starts in the rectum. These are both part of the digestive system. This is where food is broken down to make energy and where the body gets rid of solid waste (poop or stool). In the picture above you can see where the colon and rectum are inside the body.
In most cases, colon and rectal cancers grow slowly over many years. We now know that most of those cancers begin as a growth called a polyp (PAH-lip). Taking out the polyp early may keep it from turning into cancer.
Are there different kinds of colon and rectum cancers?
There are a few kinds of colon and rectum cancers.
The most common kind is called adenocarcinoma (AD-uh-no-KAR-sin-O-muh). This kind starts in the cells that make mucus to cover
the inside surfaces of the colon and rectum.
How does the doctor know I have colorectal cancer?
Some signs of colorectal cancer are changes in your poop, bleeding, and belly pain. If signs are pointing to cancer, more tests will be done.
Here are some of the tests you may need:
Blood tests: Certain blood tests can tell the doctor more about your overall health.
Biopsy (BY-op-see): For this test, the doctor takes out a small piece of tissue where the cancer seems to be. The tissue is checked for cancer cells. This is the best way to know for sure if you have cancer.
CT or CAT scan: Uses x-rays to make detailed pictures of your body. CT scans can be used to help do a biopsy and can show if the cancer has spread.
Ultrasound: For this test, a small wand is moved around on your skin. It gives off sound waves and picks up the echoes as they bounce off tissues. The echoes are made into a picture on a computer screen. It’s used to help find cancer and see if it has spread.
MRI scan: Uses radio waves and strong magnets instead of x-rays to make detailed pictures. MRI scans are helpful in looking at the liver and the brain and spinal cord.
Chest x-rays: X-rays may be done to see if the cancer has spread to your lungs.
PET scan: PET scans use a kind of sugar that can be seen inside your body with a special camera. If there is cancer, this sugar shows up as “hot spots” where the cancer is found. This test looks at the whole body. It can help if the doctor thinks the cancer has spread, but doesn’t know where.
How serious is my cancer?
If you have colon or rectal cancer, the doctor will want to find out how far it has spread. This is called staging. You may have heard other people say that their cancer was “stage 1” or “stage 2.” Your doctor will want to find out the stage of your cancer to help decide what type of treatment is best for you.
The stage describes the growth or spread of the cancer through the layers of the wall of the colon or rectum. It also tells if the cancer has spread to nearby organs or to organs farther away.
Your stage can be stage 0, 1, 2, 3, or 4. Stage 0 is also called carcinoma in situ (KAR-sin-O-ma in SY-too). The lower the number,
the less the cancer has spread. A higher number, such as stage 4, means a more serious cancer that has spread. For most people, the stage is not known until after surgery, so your doctor may wait until then to tell you about your stage and what it means for you.
Grading colorectal cancer
The cancer cells in the biopsy sample will be given a grade. This helps doctors predict how fast the cancer is likely to grow and spread. The grade is based on how much the cancer cells look like normal cells. Grades 1, 2, 3, and 4 are used. Cells that look very different from normal cells are given a higher grade (4) and tend to grow faster. Ask the doctor to explain the grade of your cancer. The grade helps the doctor decide which treatment is best for you.
What kind of treatment will I need?
There are many ways to treat colon and rectal cancers, but the main types of treatment are surgery, radiation, chemotherapy, and targeted therapy.
Two or more types of treatment may be used at the same time, or they may be given one after the other. The treatment plan that’s best for you will depend on:
- The stage and grade of the cancer
- The chance that a type of treatment will cure the cancer or help in some way
- Your age
- Other health problems you have
- Your feelings about the treatment and the side effects that come with it
Surgery for colon cancer
Most people with colon cancer have some type of surgery (SUR-jur-ee). The cancer, a small part of normal colon on either side of the cancer, and nearby lymph (limf) nodes are often removed. The 2 ends of the colon are then put back together.
For most colon cancers, an opening on the belly to get rid of body waste (poop) is not needed, but sometimes one is used for a short time. This opening is called a colostomy (kuh-LAHS-tuh-me). If you need a colostomy for a short time, your doctor or nurse can tell you more about how to take care of it and when it can come out.
Surgery for rectal cancer
Most people with rectal cancer need surgery (SUR-jur-ee). Radiation and chemo might be given before surgery. Sometimes the cancer can be removed through the anus, without cutting through the skin. This might be done to remove some stage 1
cancers that are small and close to the anus.
If the rectal cancer is more advanced and close to the anus, surgery will be done to take out the cancer and make an opening on your belly to get rid of body waste (poop). This is called a colostomy (kuh-LAHS-tuh-me). You will need it for the rest of your life.
If the rectal cancer has spread into nearby organs, more surgery is needed. The doctor may take out the rectum and nearby organs, like the bladder, prostate, or uterus, if the cancer has spread to those organs. You will need a colostomy after that surgery. If the bladder is removed, an opening to collect urine or pee (called a urostomy [yur-AHS-tuh-me]) is needed, too.
If you have a colostomy or a urostomy, you will need to learn how to take care of it. Nurses with special training will see you before and after surgery to teach you what to do.
Ask your doctor what type of surgery you will need. Ask what your body will look like and how it will work after surgery.
Side effects of surgery
Any type of surgery can have risks and side effects. Ask the doctor what you can expect. If you have problems, let your doctors know. Doctors who treat people with colon and rectal cancer should be able to help you with any problems that come up.
Radiation treatment
Radiation (RAY-dee-A-shun) uses high-energy rays (like x-rays) to kill cancer cells. After surgery, radiation can kill small spots of cancer that may not be seen during surgery. If the size or place of the cancer makes surgery hard to do, radiation may be used before the surgery to shrink the tumor. Radiation can also be used to ease some problems caused by the cancer.
For rectal cancer, radiation is given to help keep the cancer from coming back in the place where it started. It’s also used to treat cancer that has come back and is causing problems, like pain. Sometimes the radiation is aimed through the anus to reach the rectum, or small radioactive pellets or seeds might be used. They can be put around or right into the cancer. This is called brachytherapy (BRAKE-ee-THER-uh-pee).
Sometimes, both types of radiation are used.
Side effects of radiation treatments
If your doctor suggests radiation treatment, talk about what side effects might happen. The most common side effects of radiation are:
- Skin changes where the radiation is given
- Feeling sick to your stomach
- Diarrhea, pain when pooping, or blood in the poop
- Having to pee a lot, burning when you pee, or blood in the pee
- Feeling very tired (fatigue, which is pronounced fuh-TEEG)
Most side effects get better after treatment ends. Some might last longer. Talk to your cancer care team about what you can expect during and after treatment.
Chemo
Chemo (KEY-mo) is the short word for chemotherapy (pronounced KEY-mo-THER-uh-pee) — the use of drugs to fight cancer. The drugs may be given through a needle into a vein or taken as pills. The drugs go into the blood and spread through the body.
Chemo is given in cycles or rounds. Each round of treatment is followed by a break. Most of the time, 2 or more chemo drugs are given. Treatment often lasts for many months.
Chemo after surgery can help some people live longer. It can also help ease symptoms caused by the cancer.
Side effects of chemo
Chemo can make you feel very tired, sick to your stomach, and cause your hair to fall out. But these problems go away after treatment ends.
There are ways to treat most chemo side effects. If you have side effects, talk to your cancer care team so they can help.
Targeted drugs
Targeted drugs attack the changes in cells that cause cancer. These drugs affect mainly cancer cells and not normal cells in the body. They may work even if other treatment doesn’t. These drugs have different side effects than chemo, and they are often not as bad.
Side effects of targeted drugs
Side effects of targeted therapy depend on which drug is used. These drugs might cause high blood pressure, low blood counts, heart problems, and liver problems.
There are ways to treat most of the side effects caused by targeted drugs. If you have side effects, talk to your cancer care team so they can help.
What about other treatments that I hear about?
When you have cancer you might hear about other ways to treat the cancer or treat your symptoms. These may not always be standard medical treatments. These treatments may be vitamins, herbs, diets, and other things. You may wonder about these treatments.
Some of these treatments are known to help, but many have not been tested. Some have been shown not to help. A few have even
been found to be harmful. Talk to your doctor about anything you’re thinking about using, whether it’s a vitamin, a diet, or anything else.
Questions to ask the doctor
- Why do you think I have cancer?
- Do you know the stage and grade of the cancer?
- What will happen next?
What will happen after treatment?
You’ll be glad when treatment is over. But it’s hard not to worry about cancer coming back. Even when cancer never comes back, people still worry about it. For years after treatment ends, you will see your cancer doctor. At first, your visits may be every few months. Then, the longer you’re cancer-free, the less often the visits are needed.
Be sure to go to all of those follow-up visits. You will have exams, blood tests, and maybe other tests to see if the cancer has come back. Having cancer and dealing with treatment can be hard, but it can also be a time to look at your life in new ways. You might be thinking about how to improve your health.
You can’t change the fact that you have cancer. What you can change is how you live the rest of your life – making healthy choices and feeling as well as you can.
REFERENCES
American Cancer Society (2015) http://www.cancer.org/acs/groups/content/@research/documents/document/acspc-047079.pdf
Nzelu Abia (2015) http://guardian.ng/opinion/colon-cancer-prevention-is-achievable/
American Cancer Society (2015) Colorectal Cancer. Access: March 17th 2017, Source:
Considering complementary and alternative methods
You may hear about complementary or alternative methods that your doctor hasn’t mentioned to treat your cancer or relieve symptoms. These methods can include vitamins, herbs, and special diets, or other methods such as acupuncture or massage, to name a few.
Complementary methods refer to treatments that are used along with your regular medical care. Alternative treatments are used instead of a doctor’s medical treatment. Although some of these methods might be helpful in relieving symptoms or helping you feel better, many have not been proven to work. Some might even be dangerous.
As you consider your options, look for “red flags” that might suggest fraud. Does the method promise to cure all or most cancers? Are you told not to have regular medical treatments? Is the treatment a “secret” that requires you to visit certain providers or travel to another country?
Be sure to talk to your cancer care team about any method you are thinking about using. They can help you learn what is known (or not known) about the method, which can help you make an informed decision.
WAYS TO REDUCE YOUR CANCER RISKS
- Do not smoke. Do not use any form of tobacco.
- Take action to have a healthy body weight. Being BIG is good, but being HEALTHY is better and best.
- Be physically active in everyday life. Limit the time you spend sitting.
- Have a healthy diet:
-Eat plenty of whole grains, pulses (lentils, beans, peas and chickpeas), vegetables and fresh fruits.
-Limit high-calorie foods (foods high in sugar or fat) and avoid sugary drinks. Avoid processed meat; limit red meat and foods high in salt.
- If you drink alcohol of any type, limit your intake. Not drinking alcohol is better for cancer prevention.
- Avoid too much sun, especially for children. Use sun protection. Do not use sunbeds.
- In the workplace, protect yourself against cancer-causing substances by following health and safety instructions especially for people who work in factories and manufacturing companies.
- For women:
-Breastfeeding reduces the mother’s cancer risk. If you can, breastfeed your baby.
-Hormone replacement therapy (HRT) increases the risk of certain cancers. Limit use of HRT.
- Ensure you take part in vaccination programmes for:
-Hepatitis.
Epidemiological study reveals that 1 in every 8 persons in Nigeria is living with viral Hepatitis and about 22 million Nigerians are estimated to be infected with either HBV or HCV. 90-95% of Mother to Child Transmission of viral hepatitis ends in chronic hepatitis and in the absence of treatment, 15 – 40% of persons living with viral hepatitis will develop liver cirrhosis and/or liver cancer.
-Human papillomavirus (HPV) protect yourself against cervical
cancer.
10. Take part in organized cancer screening programmes for: Breast cancer (women), Cervical cancer (women) & Prostate cancer. Regular cancer screenings increases the chances of detecting certain cancers early, when they are most likely to be curable.
References
National Institute of Health (2015) Prevention. Access: March 18, 2017. Source: https://www.cancer.gov/research/areas/prevention
American Cancer Society (2015) Cancer prevention and detection. Accessed: March 18, 2017. Source: https://www.cancer.org/healthy.html
Cancer unlike many other diseases cannot be known with bare eyes or by mere looking at you. Cancer is not a pathogen in itself that infects the hosts and gets transmitted from one host to another. It is more correct to picture a cancer as an internal mistake of the body rather than as an external attack to our body.
For these evidence-based reasons, nobody can know that you have cancer by simply looking at you; there must be a diagnosis.
Cancer is nearly always diagnosed by an expert who has looked at cell or tissue samples under a microscope. In some cases, tests done on the cells’ proteins, DNA, and RNA can help tell doctors if there’s cancer. These test results are very important when choosing the best treatment options.
Tests of cells and tissues can find many other kinds of diseases, too. For instance, if doctors are not sure a lump is cancer, they may take out a small piece of it and have it tested for cancer and for infections or other problems that can cause growths that may look like cancer. The procedure that takes out a piece of the lump, or a sample for testing is called a biopsy.
The tissue sample is called the biopsy specimen. The testing process is sometimes referred to as pathology.
Lumps that could be cancer might be found by imaging tests or felt as lumps during a physical exam, but they still must be sampled and looked at under a microscope to find out what they really are. Not all lumps are cancer. In fact, most tumors are not cancer.
There are so many lab tests that doctors rely on to diagnose a cancer. Such as imaging procedures like: mammogram, CT scan, ultrasound, Magnetic Resonance Imaging (MRI), PET scan, X-rays, biopsy, and many others.
You may have heard from several people that they are no treatment for cancer or that cancer is not treatable, hence that once you are diagnosed with cancer; you should not worry about treating the disease. Instead, you should visit supernatural homes or healing homes for absolute cure.
This is not true. At Project PINK BLUE, we have a cancer support group, known as Abuja Breast Cancer Support Group (ABC-SG); it is made up of cancer survivors who were treated by Nigerian doctors in Nigerian hospitals.
There are many types of cancer treatment. The types of treatment that you have will depend on the type of cancer you have and how advanced it is. Some people with cancer will have only one treatment. But most people have a combination of treatments, such as surgery with chemotherapy and/or radiation therapy. You may also have immunotherapy, targeted therapy, or hormone therapy. Clinical trials might also be an option for you. However, clinical trials in cancer research are rare in Nigeria.
Cancer patients are always advised to be meticulous with their treatment and keep to appointment to avoid the advancement of the cancer.
Cancer diagnosis and treatment is usually a fascinating yet painful journey for the patient and to the family. Hence, once a patient completes treatment; there is always a huge relieve and excitement from all that are involved. The family is usually excited that they would no longer spend money on expensive chemotherapy and other treatments. But, so many cancer patients worry a lot after treatment, and they experience severe fear of the cancer coming back, which is called recurrence. Yes, you have completed your treatment, however, your doctors will want to watch you closely; you will be giving follow-up appointments and possible some tests to run from time to time.
As a cancer patient you may be eager to return to good health, work and daily life routine. But beyond your initial recovery, there are ways to improve your long-term health so that you can enjoy the years ahead as a champion.
The recommendations for cancer survivors are no different
from the recommendations for anyone who wants to improve his or her health: Exercise, eat a balanced diet, maintain a healthy weight, avoid tobacco and limit the amount of alcohol you drink.
But for cancer survivors, these strategies have added benefits. These simple steps can improve your quality of life, smoothing your transition into survivorship. Here’s what you can do to take care of yourself after cancer treatment.
Join Cancer Support Group in Nigeria
Support groups are viable platform of psychologically gaining energy and winding off depression or emotional burden associated with surviving cancer. Joining a support group near you or starting one can make a remarkable difference in your life. Cancer support group can help you to draw inspiration from others whom survived cancer years ago or younger survivors.
If you want to join a support group or start one, please contact us: call 08000CANCER or 08188 347 020. You can also email: [email protected]
Exercise
Regular exercise increases your sense of well-being after cancer treatment and can speed your recovery.
Cancer survivors who exercise may experience:
- Increased strength and endurance
- Fewer signs and symptoms of depression
- Less anxiety
- Reduced fatigue
- Improved mood
- Higher self-esteem
- Less pain
- Improved sleep
Adding physical activity to your daily routine doesn’t take a lot of extra work. Focus on small steps to make your life more active. Take the stairs more often or park farther from your destination and walk the rest of the way. Check with your doctor before you begin any exercise program. With your doctor’s approval, start slowly and work your way up.
The American Cancer Society recommends adult cancer
survivors exercise for at least 30 minutes five or more days a week. As you recover and adjust, you might find that more exercise makes you feel even better. Sometimes you won’t feel like exercising, and that’s OK. Don’t feel guilty if lingering treatment side effects, such as fatigue, keep you sidelined. When you feel up to it, take a walk around the block. Do what you can, and remember that rest also is important to your recovery.
Exercise has many benefits and some early studies suggested that it may also reduce the risk of a cancer recurrence and reduce the risk of dying of cancer. Many cancer survivors are concerned about cancer recurrence and want to do all they can to avoid it. While the evidence that exercise can reduce the risk of dying of cancer is preliminary, the evidence for the benefits of exercise to your heart, lungs and other body systems is substantial. For this reason, cancer survivors are encouraged to exercise.
Eat a balanced diet
Vary your diet to include lots of fruits and vegetables, as well as whole grains. When it comes to selecting your entrees, the American Cancer Society recommends that cancer survivors:
- Eat at least 2.5 cups of fruits and vegetables every day
- Choose healthy fats, including omega-3 fatty acids, rather than saturated fats or trans fats
- Select proteins that are low in saturated fat, such as fish, lean meats, eggs, nuts, seeds and legumes
- Opt for healthy sources of carbohydrates, such as whole grains, legumes, and fruits and vegetables
This combination of foods will ensure that you’re eating plenty of the vitamins and nutrients you need to help make your body strong.
It’s not known if a certain diet or certain nutrients can keep cancer from recurring. Studies examining low-fat diets or diets that contain specific fruits and vegetables have had mixed results. In general, it’s a good idea to eat a varied diet that emphasizes fruits and vegetables. While it may be tempting to supplement your diet with a host of vitamin and mineral supplements, resist that urge. Some cancer survivors think that if a small amount of vitamins is good, a large amount must be even better. But that isn’t the case. In fact, large amounts of
certain nutrients can hurt you. If you’re concerned about getting all the vitamins you need, ask your doctor if taking a daily multivitamin is right for you.
Maintain a healthy weight
You may have gained or lost weight during treatment. Try to get your weight to a healthy level. Talk to your doctor about what a healthy weight is for you and the best way to go about achieving that goal weight.
For cancer survivors who need to gain weight, this will likely involve coming up with ways to make food more appealing and easier to eat. Talk to a dietitian who can help you devise ways to gain weight safely.
You and your doctor can work together to control nausea, pain or other side effects of cancer treatment that may be preventing you from getting the nutrition you need. For cancer survivors who need to lose weight, take steps to lose weight slowly — no more than 2 pounds (about 1 kilogram) a week. Control the number of calories you eat and balance this with exercise. If you need to lose a lot of weight, it can seem daunting. Take it slowly and stick to it.
Stop using tobacco
Kick the habit once and for all. Smoking or using chewing tobacco puts you at risk of several types of cancer. Stopping now could reduce your risk of cancer recurrence and also lower your risk of developing a second type of cancer (second primary cancer). If you’ve tried quitting in the past but haven’t had much success, seek help. Talk to your doctor about resources to help you quit.
Drink alcohol in moderation, if at all
If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women of all ages and men older than age 65, and up to two drinks a day for men age 65 and younger. Alcohol does have health benefits in some people — for instance, consuming a drink a day can reduce your risk of heart disease. But it also increases the risk of certain cancers, including those of the mouth and throat.
While it isn’t clear whether drinking alcohol can cause cancer recurrence, it can increase your risk of a second primary cancer.
Weigh the risks and benefits of drinking alcohol and talk it over
with your doctor.
Do what you can
While you may worry that it will take an entire overhaul of your lifestyle to achieve all these goals, do what you can and make changes slowly. Easing into a healthy diet or regular exercise routine can make it more likely that you’ll stick with these changes for the rest of your life.
References
Mayo Clinic (2014) Cancer survivors: Care for your body after treatment. Accesed: March 18, 2017, Source: http://www.mayoclinic.org/diseases-conditions/cancer/in-depth/cancer-survivor/art-20044015?pg=1
Palliative care (or supportive care) is care that focuses on relieving symptoms caused by serious illnesses like cancer. It can be given at any point during a person’s illness to help them feel more comfortable.
The goal of palliative care is to prevent or treat, as early as possible, the symptoms and side effects of the disease and its treatment, in addition to the related psychological, social, and spiritual problems. The goal is not to cure. Palliative care is also called comfort care, supportive care, and symptom management.
Palliative care is given throughout a patient’s experience with cancer. It should begin at diagnosis and continue through treatment, follow-up care, and the end of life.
Hospice & Palliative Care
Although hospice care has the same principles of comfort and support, palliative care is offered earlier in the disease process. A person’s cancer treatment continues to be administered and assessed while he or she is receiving palliative care. Hospice care is a form of palliative care that is given to a person when cancer therapies are no longer controlling the disease. It focuses on caring, not curing. When a person has a terminal diagnosis (usually defined as having a life expectancy of 6 months or less) and is approaching the end of life, he or she might be eligible to receive hospice care.
As part of Union for International Cancer Control (UICC) & Pfizer funded programme, Project PINK BLUE partners with a number of palliative care and hospice homes. If you or your family member needs a hospice service or palliative care, please don’t hesitate to contact us: call 08000CANCER or 08188 347 020. You can also email: [email protected]
Palliative care in Nigeria
Nigeria is one dodgy religious country. Apart from persons caught-up with old age and did not have extended family members to take care of them, many persons who are unfortunate to be befell by terminal diseases, attribute their predicaments to being spiritual.
Such statement like, “God forbid, it is not my portion to suffer this disease”, “Holy Ghost fire”, are often heard among patients. Coupled with aboriginal philosophies, victims relent from going to visit experts. Many would rather prefer going to their religious organisations in what they call, “For divine healing”, instead of going for palliative rather than elusive curative approach. Many Nigerians, though, support this thinking, because it was said by the authorities that the toughest pain medication, which had been advocated for dealing with harsh pain in terminal illness is at-present, not readily accessible in the country.
“One major hindrance in rendering palliative care in our environment is the taboo of speaking of an impending death. There seems to be a culture of “death denial” among patients, their relatives, and healthcare professionals. The Igbo of Eastern Nigeria have a culture of celebrating life (“Ndu bu isi”), while despising and fearing death, especially if the dead was younger than 60 years. Where death is accepted, Nigerians prefer natural prolongation of the dying process and want to be at home so that they can make their peace, say farewell, and give final instructions to immediate relatives. Hence one finds that many terminally ill keep away from medical treatment for fear of hospitalization,”.
It has been reported that only six tertiary hospitals in Nigeria provides palliative care services. Clearly, more action is needed to strengthen the palliative care needs in Nigeria considering
that most people diagnosed with cancer present late stages/metastatic disease.
References
National Cancer Institute (2010) Palliative Care in Cancer. Accessed: March 19, 2017. Source:https://www.cancer.gov/about-cancer/advanced-cancer/care-choices/palliative-care-fact-sheet
Onwumere, O. (2013) Perils Of Operating Palliative Care In Nigeria. Access March, 17, 2015. Source:
http://nigerianobservernews.com/16082013/features/features7.html#.VRUDKI51zLU
In Nigeria, cancer as a non-communicable disease is yet to get a viable policy action from the Nigerian government including the federal and state government. The Nigeria’s Federal Ministry of Health (FMoH) executes cancer policy through the National Cancer Control Programme (NCCP), which is more like a cancer desk and does not have sufficient funding and capability to comprehensively control cancer in Nigeria. The burden of cancer in Nigeria is too huge to be in the auspices of a desk. So many countries across Africa and globally are taking drastic measures to reduce the burden of cancer and alleviate the pains caused by the disease. Nigeria requires a National Agency on Cancer Control, which should be under presidency in order to drastically step-up the fight against cancer in Nigeria.
Nigerian need an agency for cancer control, which will replace the cancer desk and will drive comprehensive cancer prevention, screening, palliative care, cancer registration and data generation for planning; research and service arm that would look after many centres for treatment in different teaching hospitals. The agency will be looking out for data on cancer and use the data for policy processes and will also mobilize private sectors to invest in cancer care. Federal Ministry of Health (FMoH) is upgrading seven (7) Oncology Centres of Excellence focused on comprehensive cancer care; with a plan of setting up additional seven (7) centres, totaling fourteen (14) across Nigeria.
The global best practice (shown with examples from Spain, with Institit Catalonia d’Oncologia (ICO) and Cancer Australia in Australia). The
National Cancer Control Agency will provide comprehensive cancer care, drive the upgrade of the existing treatment centres, propel access and availability of HPV vaccine, pursue a waiver of import duties for cancer medication and chemotherapy in order to get pharmaceutical companies to reduce the traumatic cost of cancer drugs, and overall coordination of cancer control just like HIV/AIDs.
Cancer control policies can only be driven if Nigerians advocate for it and consistently engage the National Assembly and the presidency to take action in cancer control in Nigeria. Hence, cancer control in Nigeria must be a collaborative effort of all Nigerians including NGOs, CSOs, cancer patients, medical practitioners, professional associations, trade unions and every human being living in Nigeria or associated to Nigeria.
NGOs/CSOs and Cancer Policy Advocacy in Nigeria
There are several cancer fighting non-governmental organizations and civil society groups in Nigeria who are doing remarkable work in the area of creating awareness, through rural medical missions, awareness walk, concerts and events, movie premieres, social media campaigns, corporate engagement and a number of other activities. Some also focused on provision of free cancer screenings, free mammograms, free ultra-sound and other screenings; while some others focused on patient’s care like fundraising for patients and psychological support and support groups.
Very few NGO/CSO are in engaged in advocacy driven projects, directed towards engaging Nigerian federal and state government to set-up policies targeted at cancer control. Ultimately, the works of NGOs/CSOs are commendable and huge, unfortunately cannot make a sustainable difference without government policies. For instance, the whole of South-south Nigeria does not have one single radiotherapy centre that is functional and this is a region with the highest federal budget allocation. Cancer fighting NGOs/CSOs need to work more in the area of policy driven advocacy.
Cancer Survivors and Cancer Policy in Nigeria
In Nigeria, there are thousands of cancer survivors across the country, but very few survivors are seen speaking and making public statements on cancer.
Cancer survivors in Nigeria decline from public appearances for a number of reasons, but stigma associated with cancer in Nigeria seems to be the most critical of all. For instance, in an interview conducted by Project PINK BLUE revealed that a cancer survivor who is married and have children might not like to publicly speak about his/her cancer journey, as some fragment of the society may label them and their children may have problem getting married and building relationships. For cancer survivors who got care in India, United Kingdom and other foreign countries, they seems to have other reasons like anger with the entire health system.
Despite all these challenges, cancer survivors are primary actors in cancer control; their voices are stronger than the voices of other advocates including the doctors. They passed through cancer and cancer passed through them. They can make a remarkable difference in cancer control in Nigeria.
Cancer survivors need to perceive cancer advocacy as a platform to give back to the society, they need help other women, they need to come out from their closest and advocate for a viable cancer control policy so that other women, children and men will not suffer as they suffered.
Are you a cancer survivor (champion), and wishes to lead advocacy in Nigeria, and you need help; please don’t hesitate to call 08000CANCER or 08188 347 020. You can also email: [email protected]
Cancer incidence has been increasing in most regions of the world, but there are huge inequalities between rich and poor countries. Incidence rates remain highest in more developed regions, but mortality is relatively much higher in less developed countries due to a lack of early detection and access to treatment facilities. For example, in western Europe, breast cancer incidence has reached more than 90 new cases per 100 000 women annually, compared with 30 per 100 000 in eastern Africa. In contrast, breast cancer mortality rates in these two regions are almost identical, at about 15 per 100 000, which clearly points to a later diagnosis and much poorer survival in eastern Africa.
Until recently, cancer has been excluded from broader discussions of global health. International and local organizations alike have focused on preventive and simple curative therapies, mostly for infectious diseases. However, as the global health community has recognized the
growing burden of cancer and other complex, chronic diseases, more organizations have realized that resources must be dedicated to creating systems that can provide the entire breadth of health services. Leadership by the Union of International Cancer Control, the Global Taskforce for Cancer Care and Control, ministries of health and many local partners have supported efforts for access to comprehensive cancer care with a focus on low and middle-income countries and equitable access to healthcare as a human right.
References
B.W. Stewart, C.P. Wild (2014), World Cancer Report 2014. Lyon: World Health Organization/ International Agency for Research on Cancer.
World Health Organization/ International Agency for Research on Cancer (2013) Latest world statistics. Lyon: WHO/IARC Press Release, 12 December, 2013.
Global RT, 2017, Source: http://globalrt.org/about-cancer/
In Nigeria and globally there have been series of misdiagnosis of cancer, which has led to preventable death or great chance of treatment. Hence, it is usually advisable to seek for a second opinion once cancer is suspected through some unclear signs and symptoms.
Due to the widely misunderstood nature of cancer, cancer misdiagnosis is among the most common type of medical misdiagnosis. Cancer misdiagnosis can have devastating results for the patient. In cases where cancer is not identified or mistaken for another disease, patients may miss a critical window for treatment. As a result, the patient may experience severe worsening of their condition or death. When another disease is misdiagnosed as cancer, the patient may undergo unnecessary painful and emotionally tolling cancer treatment. Additionally, the undiagnosed disease may be left to progress and
cause additional health complications. When misdiagnosis occurs, it can be difficult to find the necessary information to change diagnosis and the course of treatment for the patient. For these reasons, it is important for doctors and patients to explore all diagnosis options while carefully monitoring a diagnosed condition and its response to the provided treatment.
Misdiagnosis through Symptoms
A significant cause of misdiagnosis is a similarity of symptoms coupled with a lack of knowledge regarding the cause of the symptoms. For example, ovarian cancer and endometriosis may exhibit nearly identical symptoms. Both conditions can cause severe pelvic pain, diarrhea, constipation, infertility, and irregular menstrual bleeding. When doctors cannot identify significant evidence supporting one condition over the other, a misdiagnosis is more likely to occur.
Commonly Misdiagnosed Cancers
Experts believe that the most commonly misdiagnosed forms of cancer are due to the high frequency of occurrence of these cancers. Additionally, many patients may not exhibit signs and symptoms of these and other forms of cancer until their condition reaches an advanced stage. For this reason, both doctors and patients should stay vigilant and aware of symptoms, their progression or disappearance, and how they may interact with certain treatment plans.
Breast Cancer Misdiagnosis
It is estimated that one in eight women will be diagnosed with invasive breast cancer. Breast cancer may be misdiagnosed as a non-cancerous cyst, or collection of liquid contained within tissue. Inflammatory breast cancer is a type of breast cancer that causes the breast to become red, inflamed, and warm to the touch. Inflammatory breast cancer may be misdiagnosed as mastitis, or breast inflammation. Inflammatory breast cancer may also be misdiagnosed as fibrocystic breast disease, a benign condition that causes a lumpy or rope-like breast texture.
Colorectal Cancer Misdiagnosis
Colorectal cancer involves the patient’s lower intestine and rectum. Colorectal cancer may be mistaken for inflammatory bowel diseases (IBDs) such as irritable bowel syndrome (IBS) and ulcerative colitis. Colorectal cancer may also be misdiagnosed as hemorrhoids, or piles.
Pancreatic Cancer Misdiagnosis
Pancreatic cancer often causes symptoms in the patient’s digestive
tract. This can lead to misdiagnosis as conditions such as irritable bowel syndrome (IBS). Pancreatic cancer may also be misdiagnosed as gallstones or pancreatitis, or the inflammation of the pancreas. Pancreatic cancer may be diagnosed as diabetes, due to the fact that diabetes is often a symptom or risk factor of pancreatic cancer.
Lung Cancer Misdiagnosis
Lung cancer exhibits symptoms such as coughing, shortness of breath, wheezing, and a hoarse-sounding voice. These symptoms may also be present in patients who experience several types of respiratory infections and other conditions. For this reason, lung cancer may be misdiagnosed as conditions such as pneumonia, asthma, tuberculosis, or bronchitis. Lung cancer may also be diagnosed as pleurisy, which results from the inflammation of the membrane which lines the inside of the chest cavity.
Monitoring Treatment Results
In many cases, misdiagnosis is not the result of medical malpractice or doctor negligence. Cancer misdiagnosis may simply occur due to a lack of general cancer knowledge and difficulty identifying a patient’s symptoms. When misdiagnosis occurs, it can be difficult to find sufficient evidence to suggest cancer and divert the patient’s path of treatment accordingly. For this reason, it is important for doctors and patients to carefully monitor the effects of the patient’s prescribed treatment plan. Failure of treatment to alleviate symptoms and cure the patient’s condition can be a significant indicator that misdiagnosis occurred.
References
Fall (2011) Breast cancer. MPR [Hematology and Oncology Edition]: S-6(4). Academic OneFile. Web. 8 Nov. 2013.
Cunningham, David, et al. (2010) Colorectal Cancer. The Lancet 375.9719: 1030-47. ProQuest. Web. 8 Nov. 2013.
Lutschg, James H. (2009) Lung Cancer. The New England Journal of Medicine 360.1: 87-88. MEDLINE with Full Text. Web. 8 Nov. 2013.
Vincent, Audrey, et al. (2011) Pancreatic Cancer. The Lancet 378.9791: 607-20. ProQuest. Web. 8 Nov. 2013.
Paul and Perkins (2017). Disease Mistaken for Cancer. Access: March 18, 2017, Source:
http://paulandperkins.com/diseases-mistaken-cancer/
Cancer incidence has been increasing in most regions of the world, but there are huge inequalities between rich and poor countries. Incidence rates remain highest in more developed regions, but mortality is relatively much higher in less developed countries due to a lack of early detection and access to treatment facilities. For example, in western Europe, breast cancer incidence has reached more than 90 new cases per 100 000 women annually, compared with 30 per 100 000 in eastern Africa. In contrast, breast cancer mortality rates in these two regions are almost identical, at about 15 per 100 000, which clearly points to a later diagnosis and much poorer survival in eastern Africa.
Until recently, cancer has been excluded from broader discussions of global health. International and local organizations alike have focused on preventive and simple curative therapies, mostly for infectious diseases. However, as the global health community has recognized the
growing burden of cancer and other complex, chronic diseases, more organizations have realized that resources must be dedicated to creating systems that can provide the entire breadth of health services. Leadership by the Union of International Cancer Control, the Global Taskforce for Cancer Care and Control, ministries of health and many local partners have supported efforts for access to comprehensive cancer care with a focus on low and middle-income countries and equitable access to healthcare as a human right.
References
B.W. Stewart, C.P. Wild (2014), World Cancer Report 2014. Lyon: World Health Organization/ International Agency for Research on Cancer.
World Health Organization/ International Agency for Research on Cancer (2013) Latest world statistics. Lyon: WHO/IARC Press Release, 12 December, 2013.
Global RT, 2017, Source: http://globalrt.org/about-cancer/
We are delighted to share a number of resources with you; these resources were made possible through the support of our partners. Please help us to spread the word and reach more people. Feel free to download and share with your friends, colleagues, community and network.
-Breast Self Examination Guide | Click here to Download |
This awareness material helps you to learn how to examine your breast on regular basis.
-Breast Self Awareness Material (BSAM)
Breast Self Awareness Materials (BSAM) was prepared and developed by Susan G. Komen (www.komen.org). Project PINK BLUE partnered Susan G. Komen to translate the BSAM into Nigerian languages, such as Hausa, Igbo, Yoruba and Pidgin English. The goal is to bring information to Nigerians in the language they understand.
- Hausa Breast Self Awareness Material (BSAM)
- Igbo Breast Self Awareness Material (BSAM)
- Yoruba Breast Self Awareness Material (BSAM)
- Pidgin English Breast Self Awareness Material (BSAM)
- English Breast Self Awareness Material (BSAM)
-Breast Cancer Awareness Handbook | Click here to Download |
To learn about breast cancer risk, signs, symptoms, diagnosis and prevention; download this handbook.
-Cervical Cancer Awareness Handbook | Click here to Download |
To learn about cervical cancer risk, signs, symptoms, diagnosis and prevention; download this handbook.
-Prostate Cancer Awareness Handbook | Click here to Download |
To learn about prostate cancer risk, signs, symptoms, diagnosis and prevention; download this handbook.
-Advanced Breast Cancer Awareness Handbook | Click here to Download |
To learn about advanced breast cancer risk, signs, symptoms, diagnosis and prevention; download this handbook.
More information materials are coming up soon.
Please don’t hesitate to call us 08188 347 020 or write us an email: [email protected] if you have any review on the resources. At Project PINK BLUE, we are open to new ideas and criticisms.
Every year, we host series of programmes, awareness and advocacy events in Nigeria. Feel free to download our programme reports. Let us know if you desire to sponsor the next edition of any of our programmes or projects.
World Cancer Day 2015 Report | Click here to Download |
Global Day of Citizen Action 2015 Report
Pink October 2015 Report | Click here to Download |
World Cancer Day 2016 Report | Click here to Download |
World Cancer Day 2016 Brochure | Click here to Download |
Global Day of Citizen Action 2016 Report
Strategic Planning Meeting for Breast Cancer Navigation and Palliative Programme (BCNPP) Report
Sensitization Forum for Breast Cancer Navigation and Palliative Programme (BCNPP) Report
Pink October 2016 Report | Click here to Download |
Breast Cancer Navigation and Palliative Programme (BCNPP) Training Brochure | Click here to Download|
World Cancer Day 2017 Brochure | Click here to Download |
Project PINK BLUE-Health & Psychological Trust Centre sustain funding, partnerships, sponsorship, donation and impact in an effective, transparent and responsible way, by measuring impact using three major metrics:
- Cost-Effectiveness Analysis: this metric drill into our cost structure by setting a goal and evaluating if the goal was achieved or not through: the number of people whom we reached directly, patients/clients served by our patient navigators, the number of lives saved, people screened, treated and reached directly and indirectly; cancer incidence using hospital based data and online pool for awareness level.
- Social Return On Investment (S-ROI): this is our phase-to-phase or end of project reports to donors using the dimension of change and the associated impact-monitoring framework with 10 meta-indicators.
- Cost-Benefit Analysis: we quantify the ratio between the amount of money invested in our specific project and the benefit it could generate for social good-investors’ interest. We analyze what it cost not to do a project, the opportunities and what we will lose if the project fails.
Learn more about programmes through our annual reports.
Project PINK BLUE – HPTC 2015 Annual Report
Project PINK BLUE – HPTC 2016 Annual Report
- André M Ilbawi,Elizabeth Ayoo, Afsan Bhadelia, Runcie C W Chidebe, Temidayo Fadelu, and et al (2017) Advancing access and equity: the vision of a new generation in cancer control. Volume 18, No. 2, p172–175, February 2017. http://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(17)30041-4/fulltext
- Orjiako TC,,. Chidebe Runcie C.W., Okoye Ifeoma & Egwim Ndubuisi, (2017) Proactive steps towards preventing the emergence of cancer as a tropical disease: Integrating the experiences of Oncology Practitioners (2016). Presented at Research in Progress on December 14, Royal Society Tropical Medicine & Hygiene, London, UK.
- Chidebe, RCW (2016) Breast Cancer Navigation and Palliative Programme (BCNPP): Reducing the incidence of stage III or IV breast cancer in Nigeria. World Cancer Congress, Paris, France.
- Chidebe, RCW, Ekile C. (2016). World Cancer Day: Stimulating advocacies against cancer with entertainment celebrities in Nigeria. World Cancer Congress, Paris, France.
- Orjiakor CT, Chidebe, RCW & Okoye, I (2016). Caring for metastatic breast cancer patients in sub-Saharan Africa: The Experiences of Oncology Nurses.
